Multiple sclerosis and visual symptoms

Multiple sclerosis, also called ‘plaque sclerosis’, is a chronic demyelinating disease characterized by damage to myelin, a white substance that surrounds nerve fibers and modulates the transmission of action potentials in the brain.
It is one of the most common and severe chronic diseases of the central nervous system.
According to most experts, the disease is autoimmune-based, i.e. characterized by the immune system’s self-attack on the cells of the Central Nervous System and Spinal Cord.
The cause of the disease is still unknown; it is believed that there are both genetic and infectious causes. Environmental risk factors that may influence the onset of the disease are not excluded.
In 2020, the estimated number of people in the world with multiple sclerosis is 2.8 million; practically every five minutes in the world a person is diagnosed.
In Italy, around 3,600 new cases are registered each year and to date, it is estimated that around 126,000 people are affected.
Women are affected to a greater extent than men with a ratio of approximately double in prevalent cases, while among incident cases there is an average ratio of 3 women for every man affected by the disease (source: Multiple Sclerosis Barometer 2021 – Italian Multiple Sclerosis Association – AISM).
The age of onset is around 30 years and is diagnosed in young adults between the ages of 20 and 40.
The relapse and remission form accounts for around 85% of all cases and is characterized by alternating attacks or relapses, characterized by the onset of sudden neurological symptoms and phases of complete or partial remission.
The symptoms of multiple sclerosis can vary from person to person. The most recurrent effect are vision, motor activities, sensitivity disorders, depression, urinary retention, attention or memory disorders, and sexual disorders.
Visual disorders
Thirty percent of cases of multiple sclerosis begin with a visual disturbance, the disease can manifest itself mainly as:
- Optic neuritis (inflammation of the optic nerve)
- Diplopia (double vision)
- Nystagmus (rhythmic, involuntary oscillation of the eyes)
- Alterations in the color sense and contrast sensitivity
Retrobulbar optic neuritis (NORB)
It typically presents with sudden monocular vision loss and ocular pain in young adults, more commonly in women.
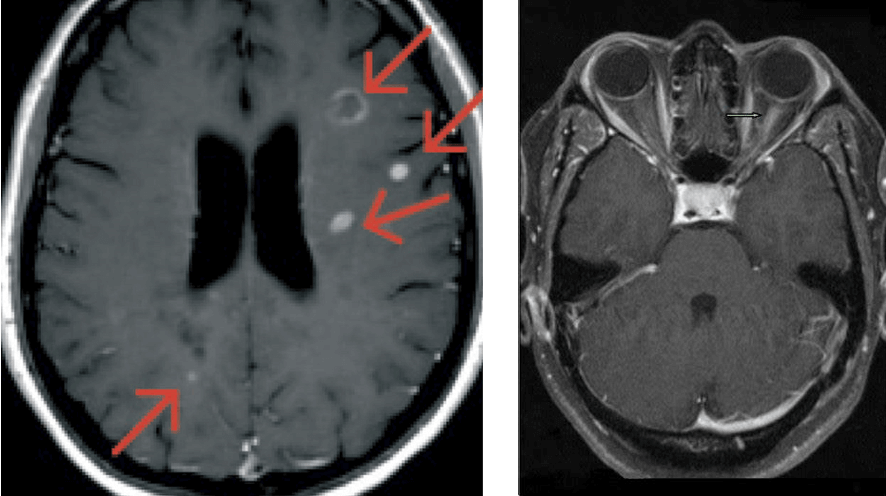
Brain Nuclear Magnetic Resonance Imaging often demonstrates white matter T2 signal abnormalities consistent with areas of demyelination (typical multiple sclerosis lesions).
The treatment of optic neuritis of choice involves the use of both intravenous and oral corticosteroids. If treated early and in the acute phase, the inflammation can recede almost completely.
The clinical assessment by the ophthalmologist is crucial.
If the patient presents with pain in eye movements and difficulty in reading, he or she should immediately go to an eye clinic to be examined.
Approximately 60 percent of patients have at least one episode of NORB throughout the disease.
Diplopia
The oculomotor changes in multiple sclerosis are linked to motor control deficits in the brain. In bilateral forms, one can mention internuclear ophthalmoplegia, where the nerve fibers that coordinate both eyes in horizontal movements are damaged.
Horizontal (lateral) eye movements are impaired, but not vertical eye movements and convergence.
These patients may present with diplopia when looking sideways, but retain single vision when looking at an object in the primary position.
In the literature, diplopia due to paresis of the 6th cranial nerve, linked to a deficit of innervation of the lateral rectus, is also very common, resulting in diplopia when the subject shifts gaze laterally.
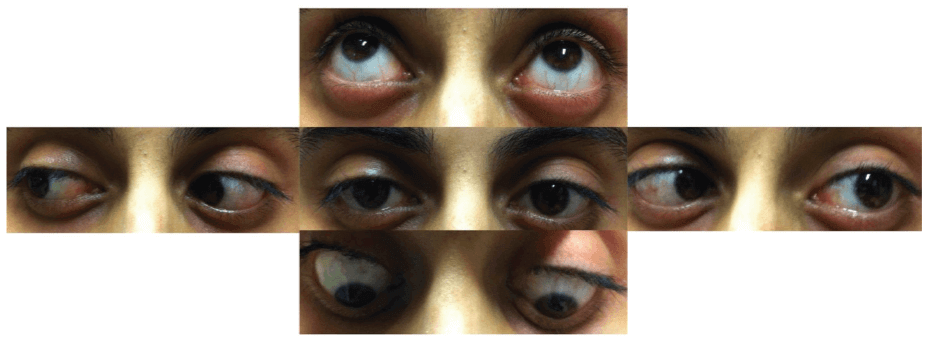
Images were taken two weeks after the onset of diplopia.
Abducens nerve paresis tends to be unilateral and restitution ad integrum (complete recovery) occurs within approximately 2-4 months, even with medication.
If diplopia occurs in the primary position, during orthoptic evaluation correlated with an instrumental examination (Hess screen) it is possible to quantify the type of paralytic squint and follow its evolution over time (follow-up).
Sclerosis and Computerized Optical Tomography (OCT)
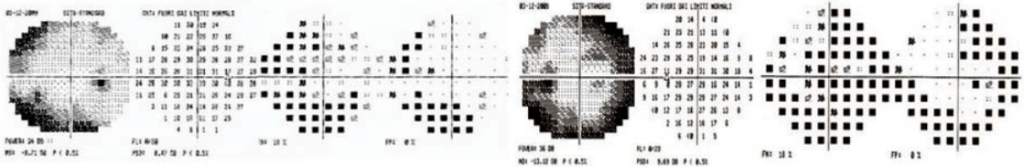
According to recent studies, a correlation has been seen between reduced OCT nerve fiber thickness and retinal ganglion cells that are closely related to reduced contrast sensitivity and color sense in affected subjects.
The pupillary response to light in patients with multiple sclerosis also appears to be related to the thinning of macular retinal ganglion cells, especially in subjects with an acute history of optic neuritis.
Conclusions
Visual disturbances affect about 1 in 4 patients and very often occur at the onset of the disease.
The ophthalmic and orthoptic examination in patients with suspected multiple sclerosis, especially at the onset, plays a key role in assessing the typical signs and symptoms of the disease.
Correct and timely diagnostic framing makes it possible to manage the signs and symptoms in the best possible way, to ensure, in agreement with the neurologist, the right therapy for the affected person.
Bibliography
- Associazione Italiana Sclerosi Multipla (AISM) – “Barometro della Sclerosi Multipla 2021” – https://agenda.aism.it/2022/
- Josefine Britze – Jette Lautrup Frederiksen – “Optical coherence tomography in multiple sclerosis” – https://www.nature.com/articles/s41433-017-0010-2
- Sundaram AN, Gelkopf MJ – “Abducens Nerve Palsy as a Presenting Symptom of Multiple Sclerosis”. Turk J Ophthalmol. 2022 Aug 25;52(4):291-294. doi: 10.4274/tjo.galenos.2022.13245. PMID: 36017545; PMCID: PMC9421932 – https://pubmed.ncbi.nlm.nih.gov/36017545/

You are free to reproduce this article but you must cite: emianopsia.com, title and link.
You may not use the material for commercial purposes or modify the article to create derivative works.
Read the full Creative Commons license terms at this page.