Rehabilitation of hemianopsia with prismatic segments

Limitations in visual field extension can have a significant impact on activities of daily living, mobility and autonomy. In addition, they can reduce the ability to avoid obstacles, increasing the risk of falls.
Prismatic lenses have been proposed for decades as a way to help people with vision problems. These include monocular vision, tunnel vision, hemianopsias, and other field-of-view alterations. Prismatic lenses bring part of the scene that cannot be seen back within the functional portion of the visual field.
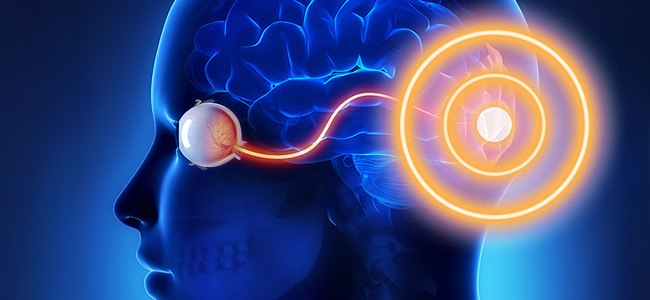
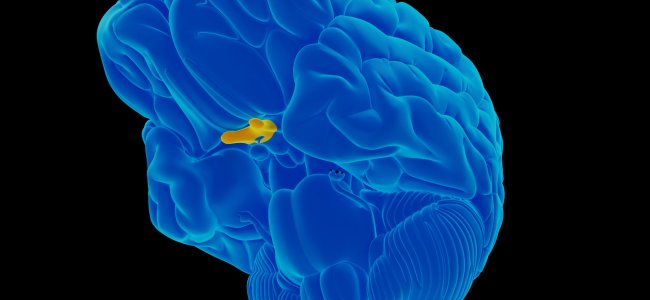
This article will focus on some rehabilitation strategies for treating complete homonymous hemianopias. In this case, the patient is unable to perceive stimuli from the right or left side of the visual field relative to both eyes.
Early approaches in history
Among the earliest approaches in this field is the use of full-field twin prisms: prismatic lenses with a base concordant to the deficient side are placed in front of both eyes, thus shifting the entire scene in the opposite direction to the unseen side.
The price of the gain on the hemianoptic side is, however, a loss of the same magnitude on the healthy side; moreover, the patient, to fixate on the stimuli coming from the hemianoptic side, has to rotate his gaze in the opposite direction, negating the normalizing function of eye movements that the rehabilitation approach should have. Monocular use is also not free of insurmountable flaws, related in particular to diplopia (the same image seen with different localisations) and confusion (different images seen in superimposition) in the center.
To partially remedy these problems, the fitting of prisms only on the portion of the lens oriented towards the side not seen by the patient has been proposed. However, this introduces a pericentral scotoma (i.e. a hidden zone from view) of considerable extent near the apex of the prism.
Peripheral segments
A valid strategy for ensuring the single central vision and limiting the experience of diplopia and confusion to peripheral areas is the use of peripheral prism segments; the type of perimetric deficit will determine the positioning of the segment and the orientation of its base.
As patients usually benefit from significant image shift, the power required is high; for reasons of technical feasibility, lightness, and lens safety, the segments are therefore made with Fresnel-type prisms (a construction method that, through the juxtaposition of adjacent prismatic portions of small size, makes it possible to achieve high dioptric powers with reduced lens thicknesses, albeit reducing the optical quality of the whole).
In the following, we will examine the solution proposed by Prof. Eliezer Peli (Schepens Eye Research Institute and Harvard Medical School), which follows the principles outlined above and whose validity has been confirmed by several clinical trials. The segments used, which can be applied in the form of an adhesive (press-on) to the lens or inserted into a housing in the lens itself, have an approximate size of 35mm x 15mm and a power of 40Δ or 57Δ, allowing for an image shift of around 20° and 30° respectively. They are normally fitted in front of the eye corresponding to the deficit side with the base facing the same side, although the possibility of bilateral fitting is permitted.
As anticipated, the segments are applied in a peripheral position to reduce the impact of diplopia and confusion phenomena: in the most frequent configuration, an upper and a lower segment are used, aligned vertically to the pupil with gaze in the primary position, i.e. when the patient is looking straight ahead.
The height at which the two segments are applied is determined by the shortest distance from the pupil that does not lead to significant diplopia/confusion in the center during walking or to significant postural changes of the head. Usually, an ideal compromise is obtained by spacing each segment 6 mm from the pupil center.
The fact that the choice of the correct positioning is made according to the patient’s walking pattern reminds us that the main application of these aids is to allow an improvement in mobility; the choice of applying both segments or only one of the two also depends on the type of obstacles the patient is most likely to encounter in daily life. The aid is not, however, indicated for use when performing static tasks and reading.
The use of Peli’s prismatic segments can increase vision in terms of visual field extension as measured by binocular perimetry, but their effectiveness depends on the accompanying rehabilitation program. There is evidence showing an advantage over a placebo in some randomized and large-scale studies.
First of all, the patient must be instructed to always look through the prism-free zone of the lens: the action of the prism segments must remain peripheral and consists of superimposing on the main image a second portion (peripheral confusion) from the blind portion of the visual field, capable of alerting the patient to the approach of some obstacle or stimulus of interest to him (Figure 1).
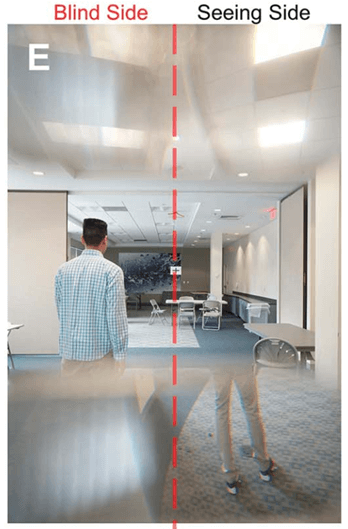
This stimulus will eventually be sought not by looking through the prism, but by moving the head and eyes so that the non-prism area of the lens is always used for central vision.
Since the prism suggests an incorrect position of the stimulus, another step in rehabilitation is to instruct the patient to compensate for this error. This is done repeatedly with gaze and touch so that the stimulus is attributed to its correct position.
Finally, the patient must be accompanied in a familiarisation phase in the use of the aid during walking, even in the presence of obstacles and steps.
Often the rehabilitation phases described above are carried out first with the upper segment only, postponing the application of the lower segment, which may involve less immediate adaptation. Since small changes in the positioning of the prismatic segments may have to be implemented and for other factors, including economic ones, it is preferable to proceed with the press-on segments in the first phase and, after at least 6 weeks of adaptation, to assess the appropriateness of more optically performing definitive solutions.
In conclusion
I segmenti prismatici periferici rappresentano una valida strategia riabilitativa nelle emianopsie e risolvono alcune delle problematiche legati ad approcci con lenti prismatiche più antiquate.
Starting with the prism segments just described, other solutions have been introduced and are being further studied to allow, for example:
- the use while driving – where this is permitted for subjects with visual field limitations of the described magnitude – with an oblique orientation of the prism base to allow a better view of the windscreen area;
- a wider image shift, for the detection of more peripheral stimuli, utilizing different optical solutions (such as multi-periscope prisms).
It is concluded by pointing out that this approach is an excellent example of how, in the use of optical aids in low vision, the best result can only be achieved when the optical study of the aid, the prescription and the rehabilitation and training phase are harmonized with each other.
Essential Bibliography
- E. Peli, “Field expansion for homonymous hemianopia by optically-induced peripheral exotropia”, Optom. Vis. Sci. 77(9), 453–464 (2000)
- R. G. Giorgi, R. L. Woods, and Eli Peli, “Clinical and Laboratory Evaluation of Peripheral Prism Glasses for Hemianopia”, Optom. Vis. Sci., 86(5), 492–502 (2009)
- H. L. Apfelbaum, N. C. Ross, A. R. Bowers, and E. Peli, “Considering apical scotomas, confusion, and diplopia when prescribing prisms for homonymous hemianopia”, Transl. Vis. Sci. Technol. 2(4), 2 (2013)
- A. R. Bowers, K. Keeney, and E. Peli, “Randomized crossover clinical trial of real and sham peripheral prism glasses for hemianopia”, JAMA Ophthalmol. 132(2), 214–222 (2014)
- C. F. Alberti, E. Peli, and A. R. Bowers, “Driving with hemianopia: III. Detection of stationary and approaching pedestrians in a simulator”, Invest. Ophthalmol. Vis. Sci. 55(1), 368–374 (2014)
- E. Peli, A. R. Bowers, K. Keeney, and J. H. Jung, “High-power prismatic devices for oblique peripheral prisms”, Optom. Vis. Sci. 93(5), 521–533 (2016).
- E. Peli, H. Apfelbaum, E. L. Berson, and R. B. Goldstein, “The risk of pedestrian collisions with peripheral visual field loss”, J. Vis. 16(15), 5 (2016)
- J.-H. Jung and E. Peli, “No useful field expansion with full-field prisms,” Optom. Vis. Sci. 95(9), 805–813 (2018)
- K. E. Houston, E. Peli, R. B. Goldstein, and A. R. Bowers, “Driving with hemianopia VI: Peripheral prisms and perceptual-motor training improve blind-side detection in a driving simulator”, Transl. Vis. Sci. Technol. 7(1), 5 (2018)
- C. Qiu, J.-H. Jung, M. Tuccar-Burak, L. P. Spano, R. B. Goldstein, and E. Peli, “Measuring the effects of prisms on pedestrian collision detection with peripheral field loss”, Transl. Vis. Sci. Technol. 7(5), 1 (2018)
- E. Peli, “Peripheral Prisms for Visual Field Expansion: A Translational Journey”, Optom. Vis. Sci. 97(10), 833-846 (2020)
- E. Peli, F. Vargas-Martin, N. M. Kurukuti, and J.-H. Jung, “Multi-periscopic prism device for field expansion”, Biomed. Opt. Express 11, 4872–4889 (2020)
- J.-H. Jung, N. M. Kurukuti, and E. Peli, “Photographic Depiction of the Field of View with Spectacles-mounted Low Vision Aids”, Optom Vis Sci. 98, 1210–1226 (2021)

You are free to reproduce this article but you must cite: emianopsia.com, title and link.
You may not use the material for commercial purposes or modify the article to create derivative works.
Read the full Creative Commons license terms at this page.