Stroke: what happens to eyesight?

Stroke can affect adults and children, with devastating consequences on health.
Body paresis and difficulty in speaking (aphasia) are the most well-known symptoms; less well known are the effects of stroke on eyesight.
Doctors themselves may underestimate the visual consequences of stroke1, and better information could promote earlier diagnosis and more effective treatment.
Intentional stroke prevention guidelines consider information essential, in part to reduce the significant commitment of care resources.
Stroke Blue Code: the 90 minutes that save lives
According to the World Health Organization (WHO), stroke is a leading cause of death and disability. Worldwide, there are an estimated 12 million cases of stroke yearly2, of which 200,000 are new cases in Italy, about 80 percent3.
All strokes are different, as are their effects and clinical diagnosis.
Ask to smile: mouth pulls to one side, is asymmetrical.
Ask to put both arms forward: one of them falls down.
Ask to repeat a simple sentence (e.g., “the sky is blue”). Cannot do it well and speaks gibberish.
Check whether the person sees blurred, does not see half of the objects, or sees double.
Figure 1 – You can recognize a stroke if one or more of these symptoms suddenly appear4.
The presence of visual impairment as the main symptom can produce a variety of possible misdiagnoses, such as a severe headache (migraine). This is compounded by the fact that 30% of people think they should go independently to the hospital at the onset of stroke5, or call their doctor (83%), instead of immediately calling the emergency numbers, dialing either 112 (used in Europe and parts of Asia) or 911 (used mostly in the Americas) .
This can delay diagnosis by several days1, compared with the 90 minutes within which a stroke victim should receive medical care, to increase survival and reduce disabling consequences.
Never underestimate a stroke, because the resulting visual problems are often mistaken for migraines, and it can take days before you realize it is not a severe headache.
An untreated ischemic stroke destroys 1.9 million neurons per minute, 13.8 billion synapses and 12 km of myelin fibers6. Compared with the normal rate of neuron loss in cerebral aging, the stroke-affected brain ages 3.6 years each hour without treatment7. Therefore, the time factor is crucial in saving the brain, but so is correct information.
Unfortunately, 80 percent of under-45s overlook its symptoms because they are convinced that the problem only affects the elderly.
How can a stroke affect my eyesight?
58% of people have eyesight problems after a stroke8, severely affecting daily life.
You may see blurry or not see half of objects (hemianopia), or see double (diplopia), in one or both eyes.
A stroke can damage any segment of the neural pathway that connects the eyes to the brain or a section of the brain that processes the images that the eyes send to it.
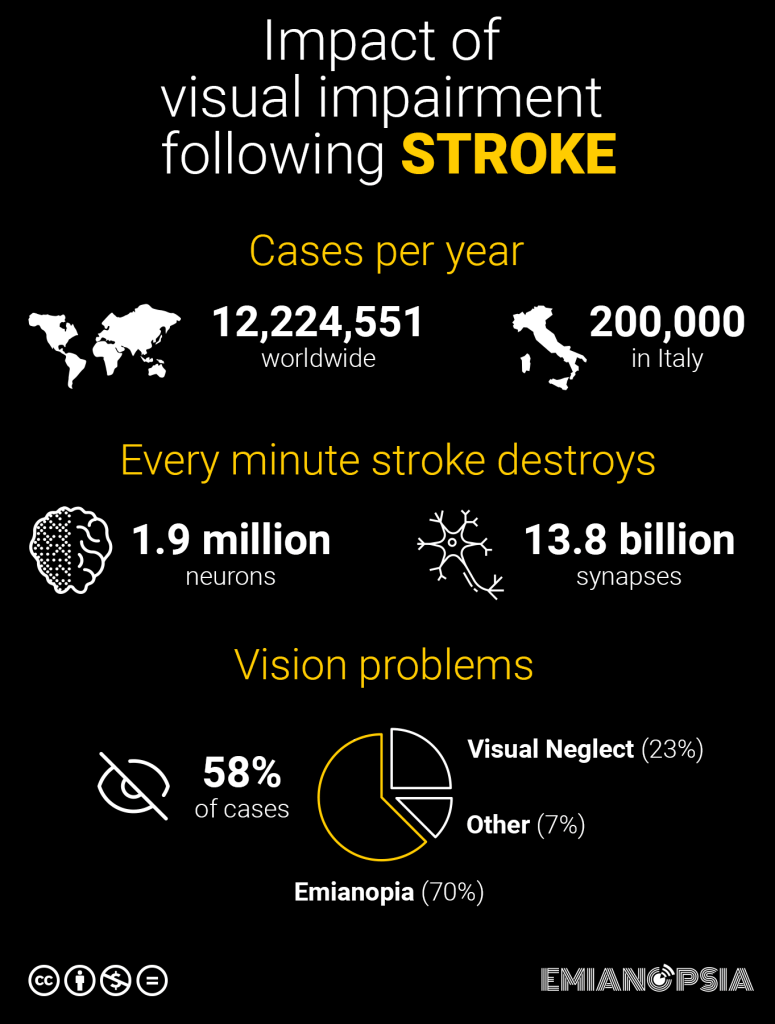
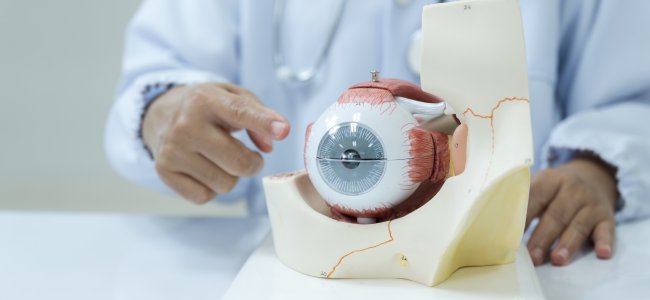
Figure 2 – Vision problems after stroke (infographic).
Hemianopia: a common loss of vision from a stroke
An epidemiological study9 has categorized the most common eyesight problems that can afflict us after a stroke.
Partial or complete loss of the visual field, in one or both eyes, is one of the most common visual problems after a stroke.
This condition is called hemianopia and requires specific rehabilitation to help the person deal with the change in visual field.
Ischemic stroke is the most common cause of hemianopia (69.7%)10, which also affects children in 25% of cases10.
For example, in Italy, 60 percent of stroke survivors develop hemianopia11.
Fifty percent of people13 with homonymous hemianopia (HH) heal spontaneously in the first month, whereas after 6 months the hemianopia becomes chronic.

Figure 3a – Simulation of right hemianopia.

Figure 3b – Simulation of left hemianopia.

Figure 3c – Simulation of superior hemianopia.

Figure 3c – Simulation of inferior hemianopia.
Partial loss of vision ability affects depth perception and the ability to judge distances. People with hemianopia have problems moving in busy environments, walking in a straight line, driving and performing visual tasks, such as helping their children with schoolwork.
Seeing food on the plate, reading, writing or watching a movie at the cinema are some of the difficulties that patients with hemianopia face daily.
In addition to the risk of tripping, falling down stairs, and possible psychological problems.
Post-stroke hemianopia, what to do?
Once past the acute phase of stroke, a rehabilitation course can be followed so as to improve lost visual function as much as possible.
After a stroke, our brain cannot grow new cells to replace those that have been damaged, but has the ability to rearrange undamaged ones and compensate for what has been lost. This is called neuroplasticity.
You can go to an ophthalmologist, orthoptist or neurologist who specializes in stroke and low vision.
They can give you an accurate diagnosis and arrange treatment for your vision issue, whether it is hemianopia, quadrantanopia, or visual neglect.
Ideally this assessment should take place before leaving the hospital, but you may be referred later to a Rehabilitation Center for the Visually Impaired.
Hemianopia is diagnosed after a thorough visual and neurological evaluation. Computerized visual field, perimetry test and MRI help define, identify, and localize the site and nature of the brain lesion. Essential investigations to begin appropriate treatment to improve residual visual ability function.
Rehabilitation of hemianopia and visual neglect
Visual rehabilitation after a stroke is possible, although until a few years ago it was believed that lesions to the primary cortex were impossible to heal.
Visual rehabilitation in patients with hemianopia or visual neglect aims to maximize residual vision and restore the maximum degree of independence in occupational and other daily activities. Thus reducing functional disability.
Precise clinical evaluation is the basis for the initiation of rehabilitation, because only by knowing exactly the type and extent of one’s injury can we adopt the most efficient therapeutic-rehabilitative program.
Visual rehabilitation requires multidisciplinary team and the creation of a personalized project, including a path capable of following the possible psychological implications.
The rehabilitation process is independent of the extent of the lesion or the time that has passed since the stroke that caused the hemianopia.
Naturally, no treatment can remove the problem that caused the hemianopia or visual neglect and return us to our initial healthy state. Research and technological innovation, however, are transforming the way we approach and treat these conditions.
Simple visual exercises to do even at home in your free time and the use of medical devices for rehabilitation enabled telemedicine, followed remotely by health professionals, can greatly improve the eyesight of hemianoptic patients.
Scientific studies have shown that an approach based on mix of audio and video stimulations of the visual field induces lasting improvement in hemianopia14. Our brain has the ability to “shift” activity related to a certain damaged function to another area of the brain.
This ability accompanies us since the birth and is also present in older people.
Subjects with visual neglect also respond much more to combined stimulation, because multisensory neurons respond effectively to audio-visual stimuli. This mechanism allows attention to be moved to a portion of space that, precisely because of visual neglect, is ignored.
A rehabilitation program tailor-made to your characteristics, a positive attitude and realistic expectations can get you through a condition that may seem insurmountable, but does not have to define your life.
There are resources, communities, and health professionals ready to help you meet your challenge, all along the rehabilitation journey.
Knowing the rehabilitation options available and who to contact can help patients and their families in the rehabilitation process.
Preventing stroke to prevent hemianopia
It is important to know the main risk factors of stroke and taking preventive measures can help15 to reduce the risk of hemianopia. For those at high risk of stroke (elderly, hypertensive, diabetic) it is even more so!
We can reduce the risk of stroke by following some simple tips16:
- reduce hypertension and cholesterol through a healthy diet, low in saturated fat and high in fiber
- lose excess weight
- perform physical activity regularly, including children and adolescents
- stop smoking
- limit the use of alcohol
- take all necessary drugs as prescribed and indicated by the doctor
Finally, entrust on health professionals and have regular diagnostic tests for stroke prevention.
Learn to manage stress, take time for yourself and others.
Ask your doctor about stroke risk and the direct correlation with hemianopia or visual neglect, based on your age, general health status, and the health history of your family members.
Health professionals can help you identify the most appropriate rehabilitation path for your case.
Bibliography
- Rowe FJ. Stroke survivors’ views and experiences on impact of visual impairment. Brain Behav. 2017; 7:e00778. https://doi.org/10.1002/brb3.778
- Impact of Stroke (World Stroke Organization)
- What is stroke? (A.L.I.Ce. Italia ODV)
- Italian regional information campaign in collaboration with Alice Toscana Onlus – Association for the fight against cerebral stroke.
- Code BLUE: Stroke Pathway: Strategy, Implementation Principles, and Socioeconomic Impact Analysis of the Stroke Pathway in Italy.
- Saver JL. Time is brain – quantified. Stroke. 2006 Jan;37(1):263-6. doi: 10.1161/01.STR.0000196957.55928.ab. Epub 2005 Dec 8. PMID: 16339467.
- Ibidem
- Rowe FJ, Hepworth LR, Howard C, Hanna KL, Cheyne CP, Currie J (2019) High incidence and prevalence of visual problems after acute stroke: An epidemiology study with implications for service delivery. PLoS ONE 14(3): e0213035. https://doi.org/10.1371/journal.pone.0213035
- Ibidem
- Zhang X, Kedar S, Lynn MJ, Newman NJ, Biousse V. Homonymous hemianopia in stroke. J Neuroophthalmol. 2006 Sep;26(3):180-3. doi: 10.1097/01.wno.0000235587.41040.39. PMID: 16966935.
- Visual Neglect and Hemianopia: rehabilitation through audiovisual stimuli
- Wolberg A, Kapoor N. Homonymous Hemianopsia. [Updated 2022 Jun 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK558929/
- Perez C, Chokron S. Rehabilitation of homonymous hemianopia: insight into blindsight. Front Integr Neurosci. 2014 Oct 22;8:82. doi: 10.3389/fnint.2014.00082. PMID: 25374515; PMCID: PMC4206079.
- Nadia Bolognini, Fabrizio Rasi, Michela Coccia, Elisabetta Làdavas, Visual search improvement in hemianopic patients after audio-visual stimulation, Brain, Volume 128, Issue 12, December 2005, Pages 2830–2842, https://doi.org/10.1093/brain/awh656
- Wolberg A, Kapoor N. Homonymous Hemianopsia. [Updated 2022 Jun 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK558929/
- Prevent Stroke: What You Can Do

You are free to reproduce this article but you must cite: emianopsia.com, title and link.
You may not use the material for commercial purposes or modify the article to create derivative works.
Read the full Creative Commons license terms at this page.