Hemianopsia: neuroscience and neuropsychological rehabilitation

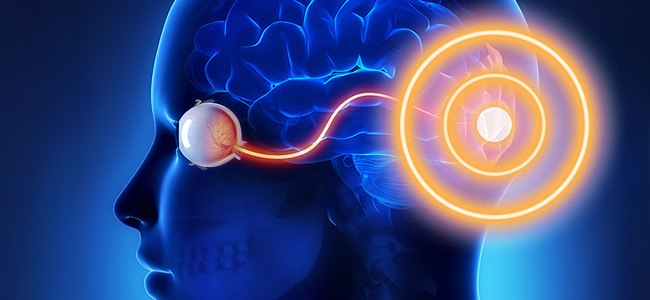
Hemianopsia is among the most frequent visual field disorders following brain damage to the primary visual pathway and manifests itself as a visual deficit in the space contralateral to the lesion.
The causes of hemianopsia can be varied, from the most common such as a stroke to a traumatic or tumor-related brain injury. The resulting disability mainly affects visual exploration, which is slow and ineffective because patients do not scan the visual field correctly.
This leads to major limitations in the activities of daily living of people suffering from hemianopsia, such as frequent bumps and falls. Moreover, as these are pathologies that often affect young people or those amid adulthood and working life, it is necessary to consider all the social and health problems associated with the situation. Therefore, the rehabilitation care of the subject with hemianopsia requires multidisciplinary teamwork and the creation of a customized rehabilitation project.
Functional assessment of the deficit and rehabilitation approaches
To structure an effective rehabilitation intervention, it is necessary to carry out a functional assessment of the deficit, through instrumental examinations and specific diagnostic protocols during an ophthalmic examination or a neuropsychological evaluation. Once the case has been framed, action can be taken to reduce the patient’s visual impairment and improve his or her quality of life using various methods. Among these, neurorehabilitation offers a scenario of interventions that can be subdivided mainly into three different approaches: substitutive, restitutive and compensatory.
The rehabilitation of hemianopsia using substitutive approaches involves the use of an external aid to restore vision in the visual field, without requiring the implementation of strategies by the patient. In this kind of sensory disorder, a substitution approach tends to be used when the use of the object is sufficient in itself to compensate for the visual problem.
In particolare, tra gli strumenti di riabilitazione sostitutivi troviamo il trattamento con gli occhiali prismatici. I prismi proiettano parte del campo visivo cieco nel campo visivo intatto con l’effetto di una possibile espansione fino al 20% del campo visivo.
For a long time, prisms were used on both eyes, but at the moment, spectacles with prisms on only one lens are preferred to increase their effectiveness and comfort of use. However, these instruments present several difficulties, such as low tolerability, which limit their use. Prisms, for example, can cause long-term problems such as the appearance of diplopia or ‘double vision’, i.e. a double representation of certain parts of the visual field.
Restitutive approach and brain plasticity
The restitutive approach, on the other hand, promotes a rehabilitation approach that aims to recover and restore the damaged function, in this case vision in the lost visual field.
Restorative rehabilitation assumes that there are still areas of residual vision.
Although there are still many open questions, more and more studies are talking about degraded but not completely blind areas, where visual capacity is present although performance is inconsistent. Generally, these areas of residual vision are found at the edges of the scotoma and can be traced back to underlying responsive areas, thus partially spared by the lesion.
During restorative rehabilitation training for hemianopsia, protocols are used involving visual detection tasks in which stimuli are presented repeatedly and intensively in the transition areas. Thus, brain plasticity mechanisms, such as synaptogenesis and synaptic potentiation, can be exploited to promote visual field restitution. Intensive stimulation and reinforcement of the connections between these areas of residual vision make it possible to expand the receptive fields of neurons and restore visual capacity.
I miglioramenti che si ottengono con i metodi restitutivi sono stabili ma i training riabilitativi difficili da attuare. Infatti, per essere individuate e stimolate le zone grigie necessitano di mappature definite ed esami del campo visivo specifici, come le microperimetrie, che sono però poco fruibili a causa dei numerosi problemi tecnici che comportano. Inoltre, i trattamenti restitutivi prevedono lunghi percorsi riabilitativi con grandi quantità di sessioni e stimolazioni ripetute e intensive.
Approccio compensativo e strategie di scanning visivo
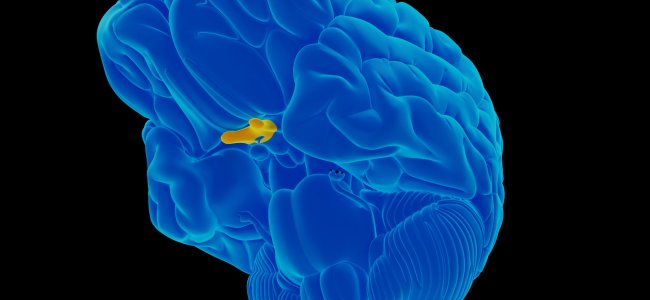
Finally, rehabilitation training with a compensatory approach attempts to develop visual scanning strategies to adapt to the deficit by exploiting alternative brain circuits spared by the lesion such as the parietal areas, frontal eye field and superior colliculi.
In general, compensatory approaches promote two types of training: top-down and bottom-up. Top-down training uses stimulation only in the visual domain and requires the patient to voluntarily and systematically scan screens in which visual stimuli appear.
In the treatment of hemianopsia, compensatory treatments have the advantage of promoting effective oculomotor strategies to compensate for the loss of a portion of the visual field. Such strategies are necessary as there is no spontaneous recovery of the deficit in hemianopsia patients.
Whereas, bottom-up training utilizes stimulation in the visual-acoustic realm. An example is multisensory visual-acoustic training which, through cross-modal visual and auditory stimulation, promotes eye movements directed toward the hemianoptic visual field. Visual-acoustic stimulation can stimulate the sub-cortical structures involved in the programming of eye movements, thus increasing the probability of detecting visual stimuli presented in the blind field.
Compensatory rehabilitation tools are effective and bring benefits that are generalized in various aspects of the daily life of the person using them.
They are generally used when restorative approaches cannot be applied or have led to few results, such as in chronic patients with low plasticity potential or significant visual field loss. Or, they can be used following restorative treatment to optimize its effects.
In conclusion
In conclusion, as the spontaneous recovery of the visual field only occurs in a small percentage of patients with hemianopsia, rehabilitation methods and tools to reduce the degree of disability play an increasingly important role in the neurorehabilitation of patients with visual field loss.
Bibliography
- B. L. Zuber, J. L. Semmlow, and L. Stark, “Frequency Characteristics of the Saccadic Eye Movement,” Biophys. J., vol. 8, no. 11, pp. 1288–1298, 1968.
- Bowers, Alex R., Egor Ananyev, Aaron J. Mandel, Robert B. Goldstein, and Eli Peli. 2014. “Driving with Hemianopia: IV. Head Scanning and Detection at Intersections in a Simulator.” Investigative Ophthalmology & Visual Science 55 (3): 1540–48. https://doi.org/10.1167/iovs.13-12748.
- C. Perez and S. Chokron, “Rehabilitation of homonymous hemianopia: insight into blindsight,” Front. Integr. Neurosci., vol. 8, no. October, pp. 1–12, 2014.
- Chedru, F., M. Leblanc, and F. Lhermitte. 1973. “Visual Searching in Normal and Brain-Damaged Subjects (Contribution to the Study of Unilateral Inattention).” Cortex 9 (1): 94–111.
- Elgin, Jennifer, Gerald McGwin, Joanne M. Wood, Michael S. Vaphiades, Ronald A. Braswell, Dawn K. DeCarlo, Lanning B. Kline, and Cynthia Owsley. 2010. “Evaluation of On-Road Driving in People with Hemianopia and Quadrantanopia.” The American Journal of Occupational Therapy: Official Publication of the American Occupational Therapy Association 64 (2): 268–78. https://doi.org/10.5014/ajot.64.2.268.
- Facchin, A., & Daini, R. O. B. E. R. T. A. (2015). Deficit centrali di campo visivo. Platform Optic, ottobre.
- Felten, D. L., & Maida, M. S. (2017, March). Atlante di neuroscienze di Netter. Edra.
- G. Kerkhoff, “Restorative and compensatory therapy approaches in cerebral blindness – a review,” Restor Neurol Neurosci, vol. 15, no. 2–3, pp. 255–271, 1999.
- G. Vallar and C. Papagno, Manuale di neuropsicologia, Terza ed. Bologna: il Mulino, 2018.
- Goodwin, D. (2014). Homonymous hemianopia: challenges and solutions. Clinical Ophthalmology (Auckland, NZ), 8, 1919.
- Goodwin, D. (2014). Homonymous hemianopia: challenges and solutions. Clinical Ophthalmology (Auckland, NZ), 8, 1919.
- Grunda, T., Marsalek, P., & Sykorova, P. (2013). Homonymous hemianopia and related visual defects: Restoration of vision after a stroke. Acta neurobiologiae experimentalis, 73(2), 237-249.
- Ishiai, Sumio, Tetsuo Furukawa, and Hiroshi Tsukagoshi. 1987. “Eye-Fixation Patterns in Homonymous Hemianopia and Unilateral Spatial Neglect.” Neuropsychologia 25 (4): 675–679.
- J. N. Carroll and C. A. Johnson, “Visual Field Testing,” 2013. [Online]. Available: http://eyerounds.org/tutorials/VF-testing/.
- J. Otero-Millan, X. G. Troncoso, S. L. Macknik, S. MartinezConde, and I. Serrano-Pedraza, “Saccades and microsaccades during visual fixation, exploration, and search: Foundations for a common saccadic generator,” J. Vis., vol. 8, no. 21, pp. 1–18, 2008.
- Kandel, E., Schwartz, J., Steven, T. M., Siegelbaum, A., & Hudspeth, A. J. (2014). Principi di neuroscienze (IV). Milano: Casa Editrice Ambrosiana.
- Làdavas, E. (2012). La riabilitazione neuropsicologica. Bologna: Il Mulino.
- Làdavas, E., & Berti, A. (2014). Neuropsicologia. Bologna: Il mulino.
- M. Rolfs, “Microsaccades: Small steps on a long way,” Vision Res., vol. 49, no. 20, pp. 2415–2441, 2009.
- N. M. Dundon, C. Bertini, E. Làdavas, B. A. Sabel, and C. Gall, “Visual rehabilitation : visual scanning , multisensory stimulation and vision restoration trainings,” vol. 9, no. July, pp. 1–14, 2015.
- Passamonti, C., Bertini, C., & Làdavas, E. (2009). Audio-visual stimulation improves oculomotor patterns in patients with hemianopia. Neuropsychologia, 47(2), 546-555. Zhang et al. 2006
- PRISMA – Bollettino Di Aggiornamento Dell’associazione Italiana Ortottisti Assistenti In Oftalmologia. Spedisce: Centro Organizzazione e Congressi, via Miss Mabel Hill 9, 98039, Taormina, Anno 2013, Numero 2
- S. Pannasch, M. Joos, and B. M. Velichkovsky, “Time course of information processing during scene perception: The ii relationship between saccade amplitude and fixation duration,” Vis. cogn., vol. 12, no. 3, pp. 473–494, Apr. 2005.
- S. Schuett, “The rehabilitation of hemianopic dyslexia,” Nat. Rev. Neurol., vol. 5, no. 8, pp. 427–437, 2009. [16] T. M. Schofield and A. P. Leff, “Rehabilitation of hemianopia,” Curr. Opin. Neurol., vol. 22, no. 1, pp. 36–40, 2009.
- Zhang, X., Kedar, S., Lynn, M. J., Newman, N. J., & Biousse, V. (2006). Homonymous hemianopia in stroke. Journal of Neuro-ophthalmology, 26(3), 180-183.
- Zihl, J. (1995a). Visual scanning behavior in patients with homonymous hemianopia. Neuropsychologia, 33(3), 287-303.
- Zihl, J. (1995b). Eye movement patterns in hemianopic dyslexia. Brain, 118(4), 891-912.

You are free to reproduce this article but you must cite: emianopsia.com, title and link.
You may not use the material for commercial purposes or modify the article to create derivative works.
Read the full Creative Commons license terms at this page.